 LEAD
LEAD In Virginia’s latest child fatality report among children who died from something other than abuse/neglect, 69.9% involved a child less than one year of age. 65.8% were related to the sleep environment (the actual surface the child slept on, with whom the child was sleeping, or how the child was sleeping). This includes children who suffocated or accidently asphyxiated due to their sleep environment.In the last fiscal year, CHIP has provided home based safe sleep education to 167 young families in our community. However, children under the age of one continue to die each month from unsafe sleep practices in our Piedmont region. How can we each take responsibility for this education and prevent unintended infant deaths?
In Virginia’s latest child fatality report among children who died from something other than abuse/neglect, 69.9% involved a child less than one year of age. 65.8% were related to the sleep environment (the actual surface the child slept on, with whom the child was sleeping, or how the child was sleeping). This includes children who suffocated or accidently asphyxiated due to their sleep environment.In the last fiscal year, CHIP has provided home based safe sleep education to 167 young families in our community. However, children under the age of one continue to die each month from unsafe sleep practices in our Piedmont region. How can we each take responsibility for this education and prevent unintended infant deaths? Shaken baby syndrome is a serious brain injury resulting from forcefully shaking an infant or toddler. Most cases are in babies less than 6 months old and are the result of a parents’ frustration over managing a baby’s crying.The lifetime cost of the United States’ Abusive Head Trauma (Shaken Baby Syndrome) cases in 2010 was an estimated $13.5 billion. Government sources (Medicaid) paid an estimated $1.3 billion. When a child survives, families, providers and caregivers can expect “a lifetime of potentially costly and life-threatening care needs.” These needs can include mobility devices, prescription medications and physical therapy.2 61 families with infants received shaken baby education in the last year at CHIP. Out-of-pocket benefits of our prevention initiative are estimated to exceed its costs if it prevents 2% of cases.
Shaken baby syndrome is a serious brain injury resulting from forcefully shaking an infant or toddler. Most cases are in babies less than 6 months old and are the result of a parents’ frustration over managing a baby’s crying.The lifetime cost of the United States’ Abusive Head Trauma (Shaken Baby Syndrome) cases in 2010 was an estimated $13.5 billion. Government sources (Medicaid) paid an estimated $1.3 billion. When a child survives, families, providers and caregivers can expect “a lifetime of potentially costly and life-threatening care needs.” These needs can include mobility devices, prescription medications and physical therapy.2 61 families with infants received shaken baby education in the last year at CHIP. Out-of-pocket benefits of our prevention initiative are estimated to exceed its costs if it prevents 2% of cases.THE HEALTH DISPARITIES SURROUNDING CHILDHOOD ASTHMA
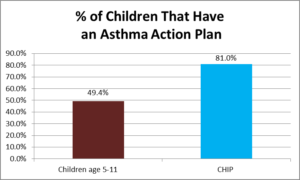
 Asthma is the leading chronic condition in children under the age of 18 with approximately 7 million suffering from asthma in the United States. However, asthma rates across socioeconomic groups and minority cultures show significant disparities.
Asthma is the leading chronic condition in children under the age of 18 with approximately 7 million suffering from asthma in the United States. However, asthma rates across socioeconomic groups and minority cultures show significant disparities.
Families with incomes below the 100 percent federal poverty line have rates of childhood asthma at 12.2 percent versus 8.2 percent in families above 200 percent of the federal poverty line.
There were approximately 629,000 ED visits for pediatric asthma for Medicaid enrollees, which cost $272 million in 2010. The average cost per visit was $433. Of the 120 children that CHIP asthma case managed over the past year, only 8 children had visits to the emergency room.
The Community Preventive Services Task Force documented studies that demonstrated savings ranging from $5.30 to $14 for every dollar invested in home-based asthma interventions focused on children and adolescents. Community-based asthma interventions, including those provided in the home, help children proactively mitigate asthma triggers and help them manage asthma symptoms throughout their daily routines [1]
[1] Nurmagambetov TA, Barnett SBL, Jacob V, Chattopadhyay SK, Hopkins DP, Crocker DD, et al. Economic value of home-based, multi-trigger, multicomponent interventions with an environmental focus for reducing asthma morbidity: a Community Guide systematic review. Am J Prev Med 2011;41(2S1):S33–S47 [PubMed]
2 Simon, A.E & Akinbami, L.J. (2016). Asthma action plan receipt among children with asthma 2-17 years of age, united states, 2002-2013. The Journal of Pediatrics. 171, pages 283-289. This article uses data from the National Health Interview Survey and is not Medicaid specific.
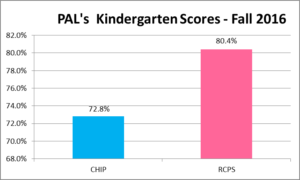
SCHOOL READINESS
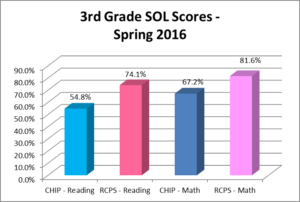
School readiness conveys important advantages. Children who enter school with early skills, such as a basic knowledge of math and reading, are more likely than their peers to experience later academic success, attain higher levels of education, and secure employment. Absence of these and other skills may contribute to even greater disparities down the road. For example, one study found that gaps in math, reading, and vocabulary skills evident at elementary school entry explained at least half of the racial gap in high school achievement scores.
CHIP caseworkers give out over 4,000 books to enrolled children each year on home visits, starting at birth, and continue until the child is discharged at first grade entry.
 |
 |
“The more that you read, the more things you will know.
The more that you learn, the more places you’ll go.”
Dr. Seuss
AFTER THE BABY IS BORN: POSTPARTUM CARE
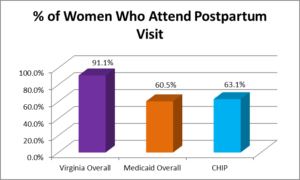
 Although it is recommended that all women undergo a comprehensive visit within the first 6 weeks after birth, as many as 40% of women do not attend a postpartum visit. In the weeks after birth, a woman must adapt to multiple physical, social and psychological changes. She must recover from childbirth, adjust to changing hormones, and learn to feed and care for her newborn. In addition to being a time of joy and excitement, this “fourth trimester” can present major challenges like lack of sleep, pain, depression, lack of sexual desire and urinary incontinence. Postpartum care visits with obstetrician-gynecologists or other obstetric care providers can help women navigate the challenges of motherhood.[i]
Although it is recommended that all women undergo a comprehensive visit within the first 6 weeks after birth, as many as 40% of women do not attend a postpartum visit. In the weeks after birth, a woman must adapt to multiple physical, social and psychological changes. She must recover from childbirth, adjust to changing hormones, and learn to feed and care for her newborn. In addition to being a time of joy and excitement, this “fourth trimester” can present major challenges like lack of sleep, pain, depression, lack of sexual desire and urinary incontinence. Postpartum care visits with obstetrician-gynecologists or other obstetric care providers can help women navigate the challenges of motherhood.[i]
[i]https://www.acog.org/…/Ob-Gyns-Stress-the-Importance-of-Postpartum-Care-The-Fourth-Trimester
 |
 |
AN OUNCE OF PREVENTION…
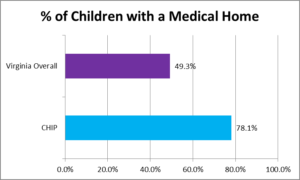
Research shows that having a medical home is associated with a reduction in health care costs. This is evident through decreased utilization of unnecessary services such as visits to the emergency department and in-patient hospitalization stays. For the pediatric population, evidence shows less out-of-pocket spending from families, particularly those with public insurance, and lower Per Member Per Month (PMPM) costs for Medicaid.
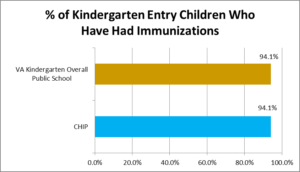
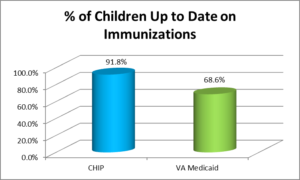
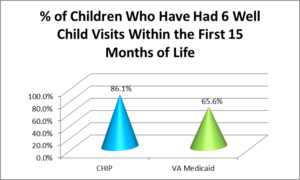
Immunization is the single most important way parents can protect their children from serious diseases. Often immunizations are given during routine well-baby visits, where doctors can pinpoint any potential medical problems or issues, should they exist, and discuss treatment options and developmental milestones with new mothers. Over the past year CHIP provided transportation for 122 well-child visits.
 |
 |
 |
PRENATAL CARE IN FIRST TRIMESTER
One of the top items on the public health agenda for the United States is access to prenatal care, particularly for low income women. In a study of low-income, inner city women in the U.S., barriers cited included lack of access to transportation to clinic appointments, denial of pregnancy to family and friends and understanding communication from healthcare systems, among others. Social workers and nurses, such as those employed through Child Health Investment Partnership, are in an ideal position to help women eliminate barriers to access to prenatal care through clinical expertise in assessment, advocacy within the health system, provision of transportation to appointments, medical records review and case management.
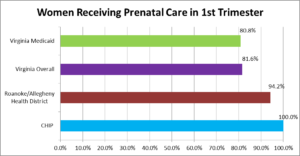
COSTS ASSOCIATED WITH LACK OF PRENATAL CARE
 According to the March of Dimes, the average length of stay for a baby admitted to the NICU is 13.2 days. The average cost of a NICU admission is $76,000 with charges exceeding $280,000 for infants born prior to 32 weeks gestation.
According to the March of Dimes, the average length of stay for a baby admitted to the NICU is 13.2 days. The average cost of a NICU admission is $76,000 with charges exceeding $280,000 for infants born prior to 32 weeks gestation.
BREAST FED IS BEST FED
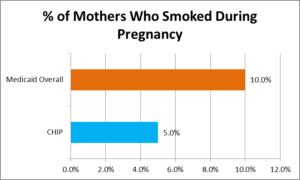
Current research shows that the practice of breastfeeding for the first 6 to 12 months of life is highly beneficial for both the mother and infant. On January 20, 2011, the United States Surgeon General released “The Surgeon General’s Call to Action to Support Breastfeeding.”[1] This report indicates that there is a 32% higher risk of childhood obesity and a 64% higher risk of type 2 diabetes for children who are not breastfed.
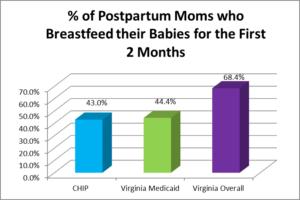
COST TO HEALTHCARE SYSTEM
The AAP says each formula-fed infant cost the healthcare system between $331 and $475 more than a breastfed baby in its first year of life. The cost of treating respiratory viruses resulting from not breastfeeding is $225 million a year.
[1] Breastfeeding and Maternal and Infant Outcomes in Developed Countries: Evidence Report/Technology Assessment Number 153, Agency for Health Care Research and Quality Publication No. 07-E007; April 2007, available at:
http://www.ahrq.gov/downloads/pub/evidence/pdf/brfout/brfout pdf.